Podcast Available on iTunes and Spotify.
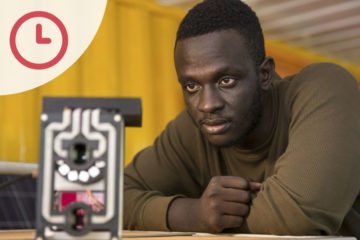
Welcome back to Five Minutes, today we’re joined by Thomas Stewart from The Mentor Initiative. He tells us about his work in malaria control.
Hi – my name is Thomas. I’m a doctor and I work as a Programme Manager for The MENTOR Initiative. We’re an organisation that for over fifteen years has provided emergency assistance against Malaria and other Vector Borne Diseases to countries, areas, and populations who are experiencing humanitarian crises.
MENTOR uses an integrated vector management approach – an evidence-based toolkit we developed in partnership with USAID, which forms the basis of our 5-day training workshops which we run a few times per year.
We’re currently operating in countries throughout sub-Saharan Africa and the Middle East, and are trusted by national governments and multinational bodies in delivering aid, health services and prevention programmes to the most vulnerable and difficult to reach populations. Research and evidence underpins everything we do and ensures that the services we provide are what is needed for the populations we serve.
The work that we do is more important than ever – despite more insecticide-treated bed nets being distributed, and more people sleeping under them, malaria cases and deaths are increasing. In 2015-16, 8 countries reported a >20% increases in malaria deaths.
So why is this happening? This is the case because of political decisions, issues involving the nets we distribute, and a lack of willingness to invest in industry to produce novel technologies that will fight the growing burden of insecticide resistance.
As a community, we are not investing enough to eliminate malaria. In May 2015, the World Health Organisation adopted the Global Technical Strategy for Malaria 2016-30, a document that laid out exactly how we can achieve a malaria-free world. This strategy states that in order to achieve this, we need $6.5 billion dollars invested in malaria annually.
To date, we are only providing $2.7 billion, just over 40% of this target. There is no doubt that this money is doing great and important work, but we clearly need to be investing a lot more.
More importantly, politically, we need a change in focus. To date, we have primarily been investing in easy win countries, those that politically stable. This often comes at the neglect of countries with protracted conflict, where international donors have little or no confidence in governments, and often for good reason. We’re talking about places where people are very vulnerable and desperate for help but governments are either not providing it, or are just not able to meet the needs alone. And unfortunately, as we at MENTOR predicted years ago, despite an increase in global prevention efforts, malaria is increasing in countries such as South Sudan and the Democratic Republic of Congo.
The people who are most in need are the ones that aren’t being helped.
Of crucial importance, the nets that the majority of malaria prevention programmes distribute are becoming increasingly unfit for purpose. In keeping with the global technical strategy, we in the malaria community are trying to reach more people at risk, but are doing so without sufficient funding increases. Basically, as we try to do more with less, quality suffers and nets which are supposed to last years are only lasting months. In addition, we are continuing to distribute pyrethroid insecticide-treated nets into areas where mosquitoes have developed resistance to this class of insecticide. It’s true that multi-country analyses have shown that these nets are still somewhat effective in this context, but continuing with this strategy will most likely worsen the growing burden of insecticide resistance.
We also need to employ more than just one tool – having a nets-only strategy is counter-productive if our goal is to truly eliminate malaria. We have the technology and capability to interrupt the mosquito at multiple stages in its lifecycle. In each malaria response, prevention programmes need a situational analysis to determine which combination of evidence-based tools will best suit the epidemiological and operational context. This is what MENTOR does in each of its programmes; we apply our Integrated Vector Management toolkit, whether it’s responding to malaria, dengue, leishmaniasis, or any other vector-borne disease.
Finally, the global community needs commercial partners to develop novel technologies that will help us reach more people and fight the growing burden of insecticide resistance. Manufacturers won’t invest in researching and producing the future tools we need if the ability to pay for a good product isn’t there.
To summarise, in the words of Dr Tedros, Director-General of the World Health Organisation,
“if we continue with a ‘business as usual’ approach – employing the same level of resources and the same interventions – we will face near-certain increases in malaria cases and deaths.”
If we, the global malaria community are realistic about eliminating malaria, we need to work in areas that are politically unstable or difficult to operate in. We need to protect these populations despite the challenges because again, these are the people who are most in need and the ones that aren’t being helped.